
Asthma Exacerbations in the Pediatric Emergency Department
J Investig Allergol Clin Immunol 2019; Vol. 29(5): 365-370
© 2019 Esmon Publicidad
doi: 10.18176/jiaci.0364
NO
2
Ozone
PM
10
30
20
15
40
40
20
50
25
60
60
30
70
80
35
One of the current hypotheses for the origin and persistence
of wheeze in children involves the interactions between
inflammatory pathways triggered by exposure to aeroallergens
and respiratory pathogens that hamper the normal development
of the airway tissues [22,23]. These changes can lead to
phenotypic alterations that probably predispose to subsequent
development of persistent wheeze [22,23]. This theory
proposes that the risk for development of persistent wheeze
and asthma is amplified if early sensitization is accompanied
by severe lower respiratory tract infections during the first
years of life [3,24].
As for infections that affect children, the prevalence of
respiratory syncytial virus (RSV) in the pediatric population
is estimated to be around 50% during the first year of life [25].
Sigurs [26] investigated the relationship between RSV and
asthma and reported a statistically significant increase in
asthma frequency in 47 children with RSV compared with
a control group. Across the world, most RSV outbreaks are
during early spring, fall, and winter [9]. More than 70% of
asthma exacerbations attended in our hospital over 1 year
are due to infections. While our findings are similar (mean
age of the sample, 3 years; highest percentage of asthma
exacerbations in the months of December, November, May,
and October), microbiological confirmation is needed in further
cohorts to clarify the origin of the infections [26].
The biological effects of pollutants and other air
contaminants such as pollen and mold spores are enhanced
in children because of the immaturity of the immune system
and physiological characteristics such as low body weight and
higher respiratory frequency [27-29]. The latter leads children
to inhale greater amounts of pollutants, with subsequent
inflammation of the smaller airways [28-29], which can
be worsened by concurrent factors, such as infection or air
pollutant peaks during pollination seasons.
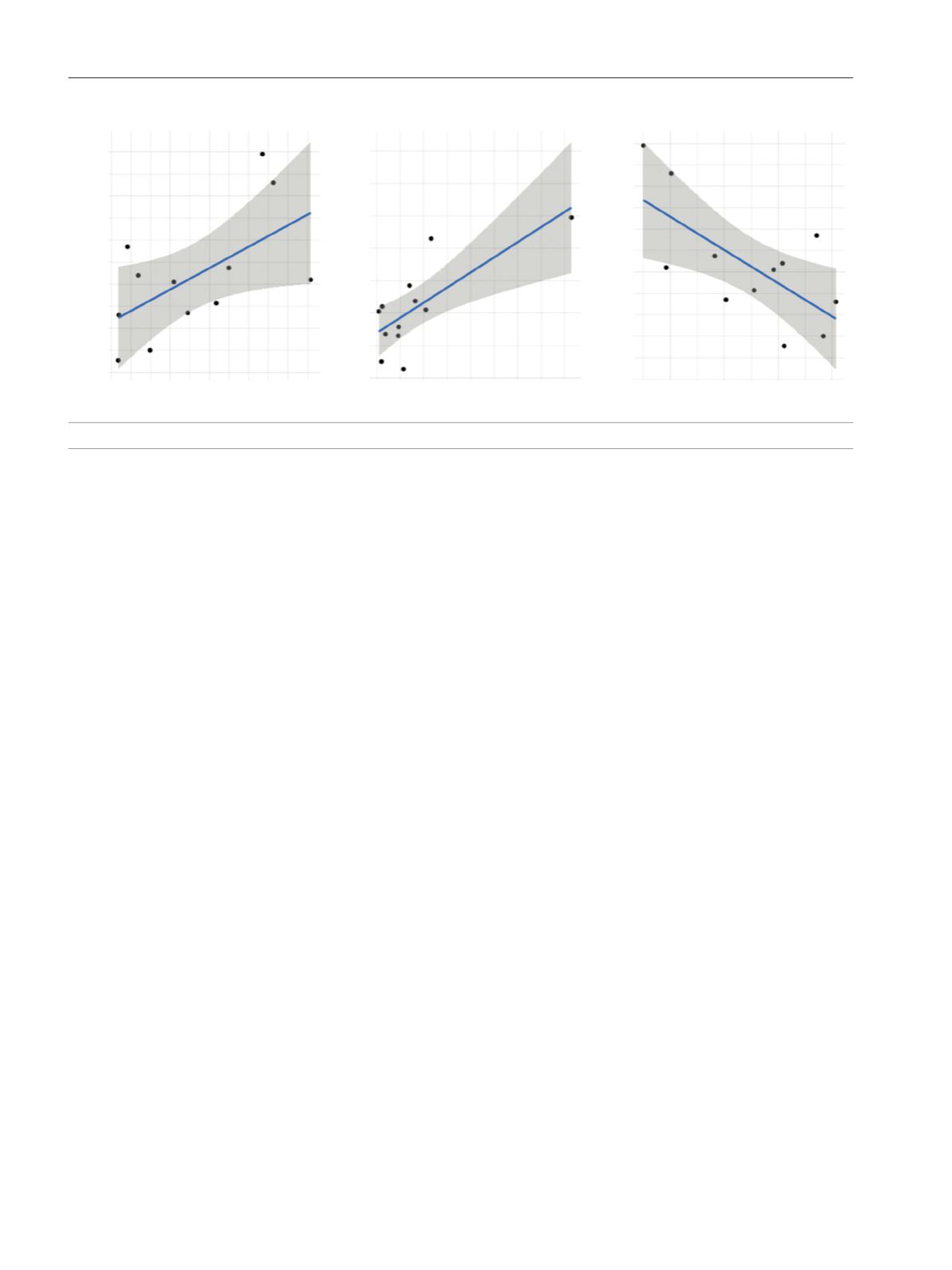
The effect of air pollution on the airway varies according
to the molecular weight of the particles. NO
2
, PM
10
, and
ozone particles have been linked to adverse effects in the
airways [17,30,31]. In our study, we found a significant
correlation between NO
2
and PM
10
and bronchospasm.
between ED admissions and PM
10
(0.028) and grass pollen
counts (0.02); (
2
) Children aged 4-7 years, who also presented
a weak correlation between ED admissions and PM
10
(0.034)
grass pollen counts (0.01); (
3
) Children aged 8-14 years, who
were affected by PM
10
, NO
2
, and ozone. We found a significant
positive correlation between them (PM
10
[0.060], ozone
[0.027], NO
2
[0.029]). Regarding pollen counts, there was a
significant though weak correlation between ED admissions
and Cupressaceae and grass pollen counts (0.011).
In more than half of the patient population, there was no
recorded follow-up by either the allergy or the pneumology
department (57.6%). Up to 11.1% of the patients were followed
up in allergy departments, 20% in pneumology departments,
and 11.2% in both. Of the admitted patients, 50.7% had regular
check-up visits by specialists (allergist or pneumologist). Of
this percentage, 22.9% were followed up by an allergist only.
Discussion
The increase in hospital admissions for wheezing or asthma
attacks is a growing health care problem in developed countries,
generating considerable costs for health systems [4,16].
Since 2016, after the Melbourne thunderstorm asthma study,
specialists around the world have been paying more attention
to ED admissions in order to detect high-risk populations [17].
In this sense, children continue to be a vulnerable population
during these types of episodes.
The treatment of asthma exacerbations is complex, since
many patients continue to have asthma-related symptoms
at home once they have been discharged from the ED [18].
The rising frequency of asthma exacerbations indicates that
management of the disease continues to be suboptimal [18-21].
In our sample, more than 20% of the children had more
than 1 asthma exacerbation in 1 year, thus reinforcing the
importance of regular check-ups and adjustment of regular
controller treatment in these patients. Adjustments should be
based on the triggers involved in the exacerbations, the medical
history, and the response to treatment in the ED.
Figure 3.
Correlation between air pollutants (NO
2
, PM
10
, ozone) and admission to the emergency department.
368
500
400
300
200
100
0
500
400
300
200
100
0
600
400
200
0
ED Admissions
ED Admissions
ED Admissions









