
Practitioner's Corner
J Investig Allergol Clin Immunol 2019; Vol. 29(5): 378-398
© 2019 Esmon Publicidad
Mepolizumab for the Treatment of Eosinophilic
Granulomatosis With Polyangiitis: Our Experience
Díaz-Campos RM
1,
*, Prudencio-Ribera VC
1,
*, García-
Moguel I
2
, Fernández-Rodríguez C
2
, Corral-Blanco M
1
, Jarrin-
Estupiñan ME
1
, Melero-Moreno C
3
1
Severe Asthma Unit. Pneumology Service, Hospital Universitario
12 de Octubre, Madrid, Spain
2
Severe Asthma Unit. Allergology Service, Hospital Universitario
12 de Octubre, Madrid, Spain
3
Institute for Health Research (i+12), Hospital Universitario 12
de Octubre, Madrid, Spain
*
These authors contributed equally to this manuscript.
J Investig Allergol Clin Immunol 2019; Vol. 29(5): 384-385
doi: 10.18176/jiaci.0407
Key words:
Asthma. Vasculitis. Eosinophilia. IL-5. Mepolizumab.
Palabras clave:
Asma. Vasculitis. Eosinofilia. IL-5. Mepolizumab.
Eosinophilic granulomatosis with polyangiitis (EGPA) is
considered a hybrid condition comprising a hypereosinophilic
disorder and systemic antineutrophil cytoplasmic antibody
(ANCA)–associated vasculitis. It is characterized by the
presence of asthma, eosinophilia, multiorgan involvement,
and, sometimes, serum ANCA [1]. Its incidence has been
reported to be 0.5 to 6.8 new cases per million habitants in
the asthmatic population [2].
Systemic corticosteroids are the first-line treatment
for EGPA. As their short- and long-term consequences are
well-known, therapy is generally with corticosteroid-sparing
immunomodulators, such as methotrexate or azathioprine [3].
Advances in knowledge of the pathophysiology of
EGPA have led to a range of new treatments, such as
omalizumab, which enables corticosteroids to be spared.
However, reducing the dose of corticosteroids can increase
the risk of severe EGPA flares [4]. Mepolizumab is an
anti–interleukin-5 (IL-5) monoclonal antibody that reduces
the absolute eosinophil count with clinical improvement in
patients with other eosinophilic disorders, such as severe
eosinophilic asthma [5].
Since the serum IL-5 level is increased in EGPA, targeted
therapy against this cytokine has proven to be an effective
alternative.
Mepolizumab has been used successfully in patients
with relapsing or refractory EGPA at an intravenous dose
of 750 mg once every 4 to 6 weeks [6,7]. In a multicenter
phase 3 study, Wechsler et al [8] administered mepolizumab
subcutaneously at 300 mg every 4 weeks and compared it with
placebo in 126 patients [8]. Since mepolizumab led to more
accrued weeks of remission than placebo, corticosteroid use
could thus be reduced. Furthermore, the time to first relapse
was longer with mepolizumab, and the exacerbation rate was
significantly lower during the treatment period than during
the nontreatment period. However, manifestations of EGPA
recurred on discontinuation [6-8]. A systematic review of the
results of these 3 studies was published in 2019 [9].
A recent post hoc analysis investigated the clinical benefit
of mepolizumab in patients with relapsing or refractory
EGPA and found that compared with the previous trial [8],
significantly more patients experienced remission or a ≥50%
reduction in corticosteroid dose or were relapse-free with
mepolizumab, mainly in specific subgroups (blood eosinophil
count ˂150/µL and weight >85 kg) [10].
We report 2 patients with corticosteroid-refractory
EGPA treated successfully with 300 mg of subcutaneous
mepolizumab every 4 weeks, according to the 2017 United
States Food and Drug Administration recommendation for
adult EGPA treatment.
A 43-year-old nonsmoking woman with a history of
allergic asthma, positive prick test results for dog epithelium
and house dust mite (
Dermatophagoides pteronyssinus,
Dermatophagoides farinae, Lepidoglyphus destructor, Blomia
tropicalis
), rhinosinusitis, and chronic suppurative otitis media
presented multiple mononeuritis, erythematous skin lesions
compatible with biopsy-proven vasculitis, and bilateral, patchy,
ground glass opacities with an upper lung distribution in a
chest computed tomography (CT) scan. Blood tests revealed
a positiveANCA titer, eosinophilia (37%), increased IgE level
(234 IU/mL), and a normal C-reactive protein level (CRP,
0.76 mg/dL). The patient was initially treated with prednisone
0.5 mg/kg/d, followed by 6 cyclophosphamide pulses (750
mg each) and azathioprine in order to spare treatment with
corticosteroids. The lowest dose reached was 10 mg/d of
prednisone, because symptoms recurred when the dose
was reduced. Omalizumab was subsequently administered
for 1 year, although it was discontinued because of lack of
efficacy (frequent asthma exacerbations and episodes of
suppurative otitis media). Subcutaneous mepolizumab was
tried at 300 mg every 4 weeks. Before starting mepolizumab
(while the patient was receiving 10 mg/d of prednisone), the
laboratory values were as follows: eosinophil blood count,
13%; serum IgE level, 234 IU/mL; and CRP, 2.07 mg/dL. The
Birmingham Vasculitis Activity Score (BVAS) was ˃3, and
FEV
1
was 103%of predicted. Sixmonths later, the asthma and otic
symptoms had improved significantly, the Asthma Control Test
(ACT) score had increased 3 points (22 to 25), blood eosinophilia
and CRP had decreased (1.1% and 0.26 mg/dL, respectively),
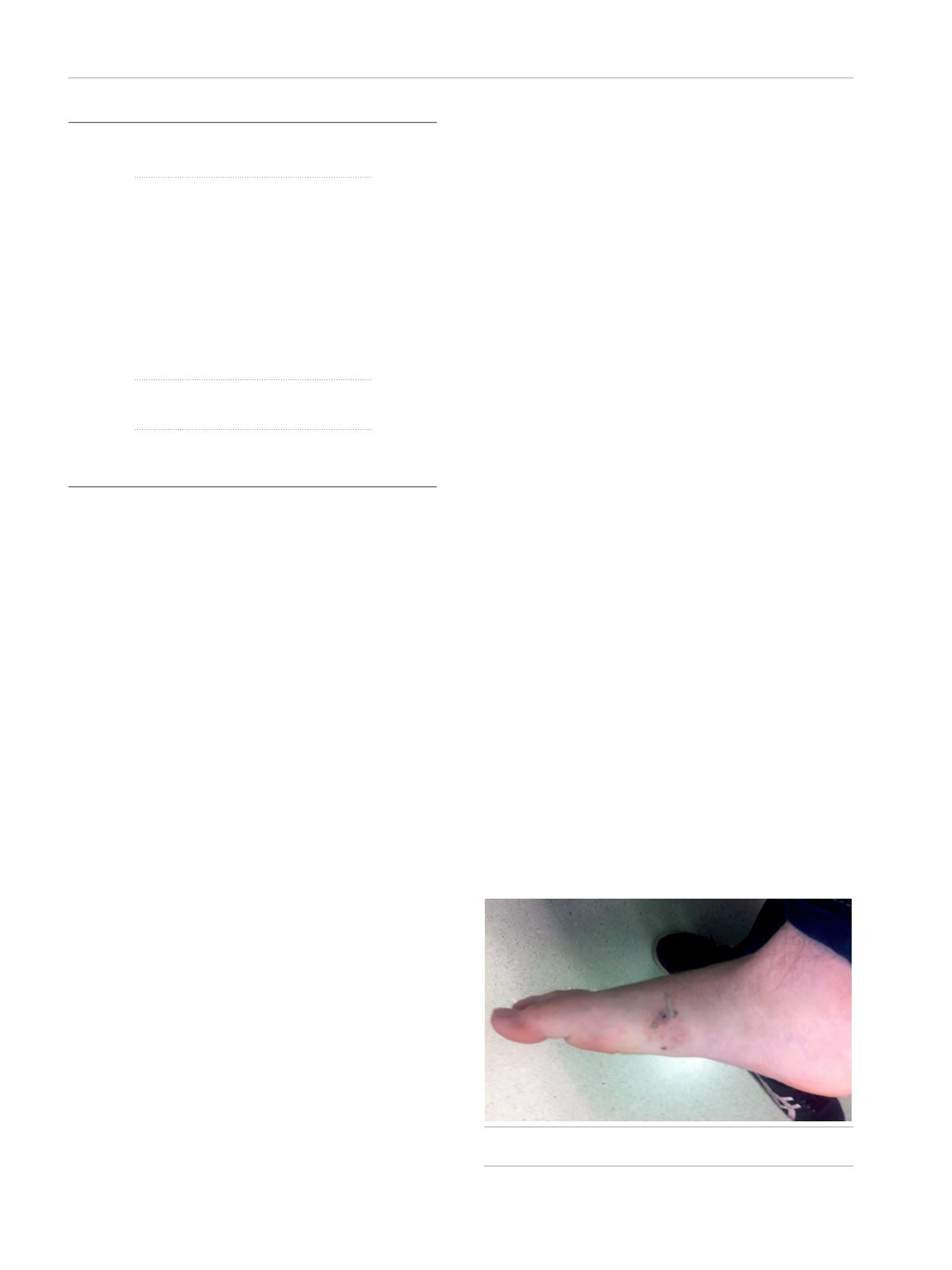
Figure.
Erythematous skin lesions in a patient with eosinophilic
granulomatosis with polyangiitis.
384









