
Neuropathic Pain/Itch in Allergic Conjunctivitis
J Investig Allergol Clin Immunol 2019; Vol. 29(5): 349-356
© 2019 Esmon Publicidad
doi: 10.18176/jiaci.0320
by capsaicin in the nasal mucosa was responsible for this
therapeutic effect. Several trials of topical capsaicin in patients
with nonallergic rhinitis have demonstrated relief of symptoms
and nasal hyperreactivity [51-53].
Systemic neuromodulating agents may constitute another
approach to the management of neuropathic symptoms in
allergic disease. With the recognition that chronic cough is
similar to other hypersensitivity neuropathic syndromes such
as chronic pain [54], gabapentin, a common treatment for
neuropathic pain, has proven clearly efficacious for refractory
cough [55]. The clinical relevance of neuroinflammation
and sensitization has also been extrapolated to chronic
itch. Cevikbas et al [56] described a synergistic role for
γ-aminobutyric acidAand B agonists for addressing symptoms
of itching in murine atopic dermatitis. The utility of gabapentin
has also been demonstrated in this setting [57].
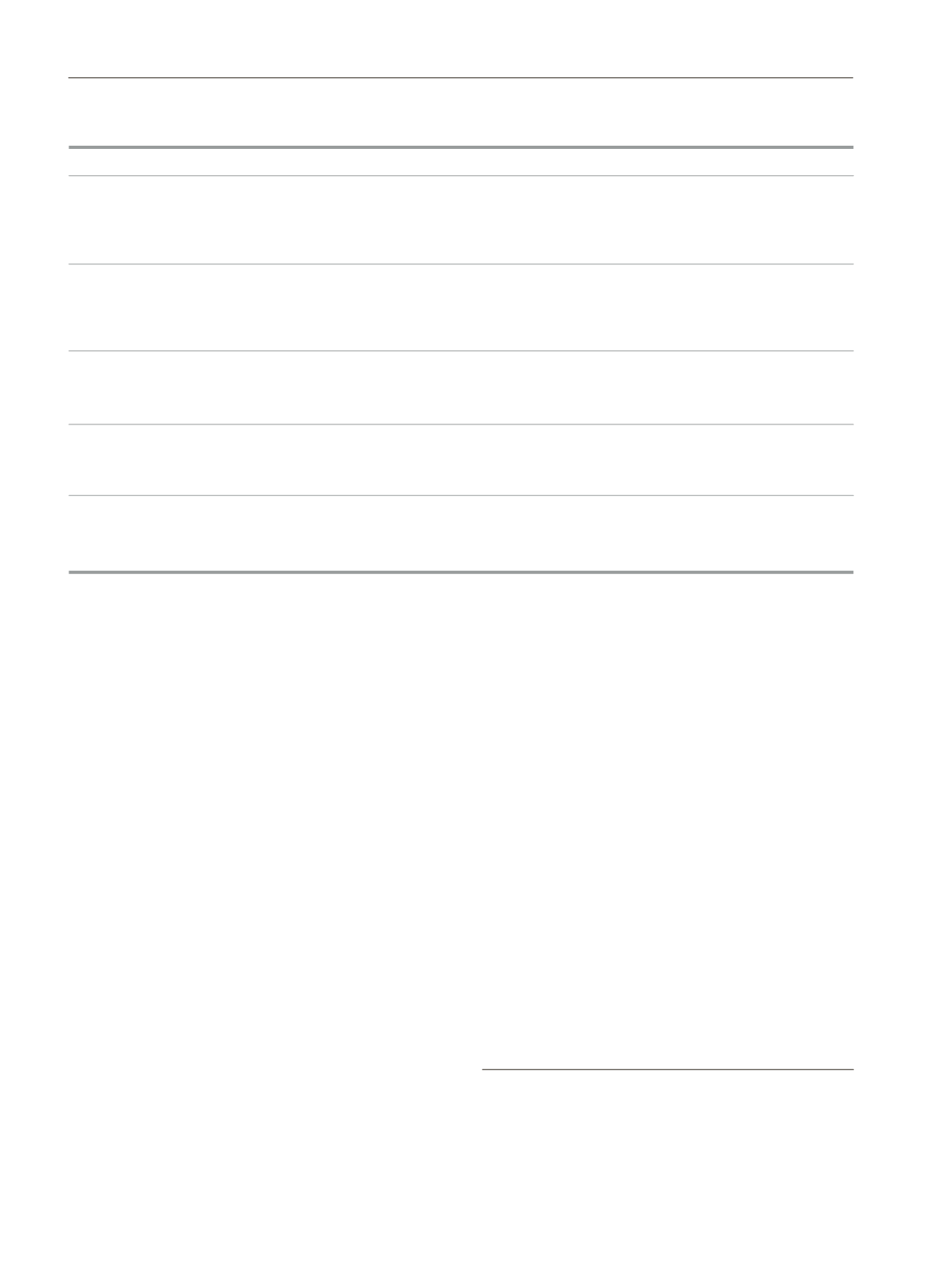
The Table summarizes trials examining neuromodulation
to date for allergic and nonallergic upper airway diseases
presumed to be related to neuroplasticity.
Future Directions
Despite substantial advances in our understanding of the
pathophysiology ofAC, the exact association between targeted
therapy and successful responses remains controversial and
prevents these findings being applied in clinical practice.
However, targeting neuronal inflammation remains a potential
novel strategy for the treatment of AC. The definition of these
pain-relevant neural circuits may facilitate future development
of targeted therapies.
Conclusions
Among the constellation of symptoms that characterizes
AC, many, such as burning and stinging, can be attributed to
chronic neuropathic pain. There is evidence to support that these
hallmark symptoms might be linked to the effects of allergen-
induced neuromodulation. Thus, neurogenic mechanisms may
have a significant role in chronic ocular surface inflammation.
Current management goals in allergic conjunctivitis aim to
minimize the inflammatory cascade associated with allergic
response in the early stages of the pathogenic mechanism.
Based on the mechanistic data reviewed herein, the recognition
that neuronal inflammation explains many of the symptoms in
AC opens new frontiers for drug discovery.
Funding
The authors declare that no funding was received for the
present study.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
1. Undem BJ, Taylor-Clark T. Mechanisms underlying the
neuronal-based symptoms of allergy. J Allergy Clin Immunol.
2014;133(6):1521-34.
2. Gomes PJ.Trends in prevalence and treatment of ocular allergy.
Curr Opin Allergy Clin Immunol. 2014;14(5):451-6.
Table.
Randomized Controlled Trials of Neuropathic Therapies for Allergic/Nonallergic Airway Inflammation
Drug
Mechanism Disease Evaluated
Outcome Assessed
Efficacy
SB-705498
Intranasal TRPV1
Allergic
Total nasal symptom score
No differences in allergen-induced
antagonist
rhinitis
(TNSS) - SB-705498 versus
mean TNSS between SB-705498
placebo, fluticasone
alone and placebo or between
propionate (FP),
SB-705498 plus FP and FP
and SB-705498 + FP
alone [49]
SB-705498
Intranasal TRPV1
Nonallergic
Total symptom score (TSS),
No differences in or maximum
antagonist
rhinitis
expressed as weighted mean
TSS at 1 hour and 24 hours
over 60 minutes (WM0-60)
postdosing on days 1 or 14,
or maximum TSS at 1 hour and
relative to placebo [50]
24 hours postdosing
Capsaicin
Intranasal TRPV1
Idiopathic
Visual analog scale (VAS) and
Significant decrease in VAS
agonist that ablates
rhinitis
therapeutic response evaluation (TRE)
and TRE scores, and abrogation
the TRPV1-SP
scores, and nasal hyperreactivity by means
of nasal hyperreactivity
signaling pathway
of cold dry air (CDA) provocation
to CDA [19]
Capsaicin
Intranasal TRPV1
Nonallergic
Visual analog scale (VAS) scores,
Significant decrease in VAS scores,
agonist that ablates
rhinitis
and nasal hyperreactivity
and abrogation of nasal
the TRPV1-SP
by means of CDA provocation
hyperreactivity to CDA up
signaling pathway
to 9 months after treatment [53]
ICX72
Intranasal TRPV1
Nonallergic Total nasal symptom scores (TNSS),
Significant improvements in TNSS
(capsicum + agonist that ablates
rhinitis
individual symptom scores (ISS)
and each ISS, and average time to
eucalyptol)
the TRPV1-SP
over 2 weeks and average time
first relief of 52.6 seconds [51]
signaling pathway
to first relief
354









